What is PPPD, or Persistent Postural-Perceptual Dizziness, and how do you treat it? How is it different from Vestibular Migraine or other vestibular disorders?
If you get daily dizziness that seems to never change, this could be an issue you face along with Vestibular Migraine. But how do doctors distinguish between the two when you have both?
Triple PD or “three PD” is a very new diagnosis that has only been recently recognized by the World Health Organization in 2017. Therefore, like most other vestibular disorders, patients may have to do some research to find a doctor that is familiar with this diagnosis. VEDA is a resource that can help.
Jump to:
Symptoms of PPPD
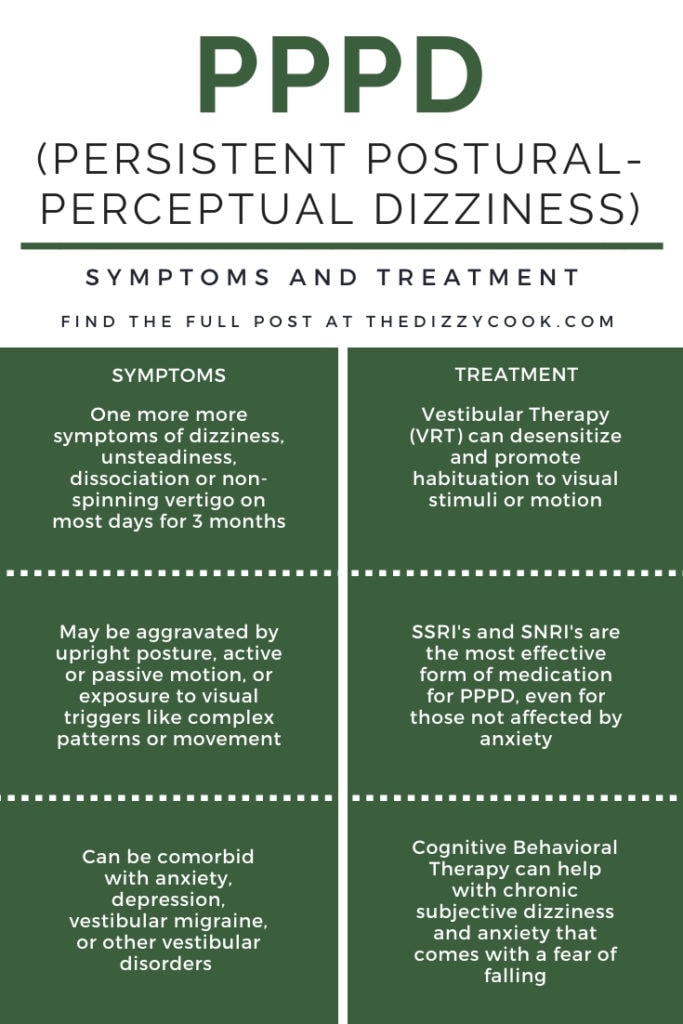
As many vestibular disorders can mimic each other, you’ll often see people question a diagnosis. PPPD, Persistent Postural-Perceptual Dizziness, is typically accompanied by symptoms of dizziness, unsteadiness, and non-spinning vertigo.
The criteria for diagnosis is that symptoms are present on most days for three months or more and can be aggravated by upright posture and increased visual stimulation through movement or complex patterns. Unlike Vestibular Migraine, which can have episodes of vertigo or intense symptoms, PPPD is a steady level of dizziness. But most often, patients have both.
Sometimes symptoms can be decreased through distraction or randomly disappear. They do not have to be continuous throughout the entire day, but can also appear for hours at a time. These episodes can originate from the brain (neurological) or be vestibular related (the inner ear). They can also come with an initial reaction of high anxiety and a fear of being suddenly imbalanced.
Some things that may increase PPPD symptoms are :
- Normal movements like standing or walking.
- Looking at traffic or any areas with movement
- Walking through a crowded grocery store
- Using a computer or phone and scrolling
- Sitting in a busy restaurant
What Causes Triple PD
This disorder can either start very obviously with an acute event, or develop slowly with a chronic event, however, the acute event is much more common. With an acute event, the symptoms might be episodic at first before becoming a pattern. There must always be a cause for PPPD to occur as it is not a stand alone diagnosis.
These acute events could be:
- Another peripheral vestibular disorder like BPPV
- A panic attack
- A neurological disorder like Vestibular Migraine
- Concussion or whiplash (perhaps from a car accident)
Chronic events could be:
- Another vestibular disorder that can be chronic like Meniere’s Disease or Vestibular Migraine
- A disease of the autonomic nervous system (or Dysautonomia)
For these events, symptoms may come on slowly and then become more persistent. See the Bárány Society diagnostic criteria for more details.
It appears that in a quarter of the cases, the event is caused by a peripheral or central vestibular disorder like BPPV or vestibular neuritis and in 20% of cases, it’s caused by vestibular migraine. (Staab JP, Eckhardt-Henn A, Horii A 2016)
How Persistent Postural-Perceptual Dizziness is Diagnosed
Bárány Society diagnostic criteria must be fulfilled so this will involve your doctor closely examining your history. Was there any major events this could be triggered by? What are the symptoms you’re experiencing and have you had them for 3 months?
Another difficult aspect is many of these symptoms crossover with vestibular migraine. You may feel a sense of motion without spinning (vertigo), have lightheadedness or a feeling like you’re swaying or “on a boat”. There’s also dissociation where you could feel like you’re floating or where you feel “out of it”. Dr. Edward Cho mentions that in his practice dissociative symptoms are actually a huge clue that PPPD is present.
Your doctor might also ask you what increases and decreases your symptoms. Do you feel worse walking in hallways with patterned carpets? Or do you search for one spot to keep yourself steady? A patient with Persistent Postural-Perceptual Dizziness may be highly dependent on visual cues.
Other vestibular tests may be performed to rule out other conditions, or help your doctor decide what other disorders coexist with PPPD. You can most definitely have BPPV and PPPD or Vestibular Migraine and PPPD. Unfortunately for some, Persistent Postural-Perceptual Dizziness is diagnosed as a catch all term when doctors have no idea how to decipher a patient’s dizziness.
The Anxiety Connection
When a patient does not use an appropriate cognitive behavioral response by thinking this is just a moment and they are safe, it adds “a secondary psychological and functional morbidity, such as fear of falling, anxiety, or depressive disorders, and functional gait abnormalities” according to research from Popkirov, Staab, and Stone. The term “gait abnormalities” basically means you walk oddly. Perhaps this is because you feel as though the ground is moving or like you’re walking on sponges. This is also a symptom of other vestibular disorders, like vestibular migraine.
While PPPD does not actually cause anxiety, anxiety and PPPD can exist closely together as a comorbidity. In fact a patient who is prone to anxiety and depression is 60% more likely to develop PPPD.
Because of the anxiety factor, many patients may need counseling as they become fearful to do certain activities and this can lead to bad habits. Not exercising, moving, or cooking(!) can be harmful in the long term.
How is PPPD Treated?
Obviously this will depend on your specific case and whether or not you’re treating a comorbidity, but the most common practices are:
- Vestibular Therapy - this is started very slowly and slightly increased with time. The idea is to reduce visual triggers and abnormal responses through movements and tasks. This promotes habituation, which allows you to be less sensitive to visual stimuli.
- SSRI’s and SNRI’s -selective serotonin reuptake inhibitors and selective serotonin norepinephrine reuptake inhibitors (typing that just did a NUMBER on my spell check…red lines all over!) seem to be the most promising medications for PPPD. You must understand that these aren’t just treating the anxiety, but actually treating PPPD. You do not have to have anxiety to benefit from this medication. However, they can also improve the comorbidity of anxiety and depression.
- In clinical practice, SSRI’s are usually started first and then SNRI’s are introduced if not effective or not tolerated well.
- SSRI’s and SNRI’s can be expected to have a response within 8-12 weeks. If these are found to be beneficial for the patient, treatment is typically continued for at least one year.
- The most popular is Effexor ER/Venlafaxine, which begins at 37.5mg for dosage. But microdosing can help mitigate side effects. This would involve a schedule of breaking open the capsule and taking a certain amount of the beads. This must be done under the guidance of a neurotologist, neurologist or ENT.
- CBT - Cognitive Behavioral Therapy - More recent studies have showed CBT can lead to up to a 75% improvement in some patients with chronic subjective dizziness, which seemed to continue at 1 and 6 months of treatment. (E J Mahoney A, Edelman S, D Cremer P. 2013). CBT can also help with the anxiety comorbidity and help patients who fear falling or the perceived risks associated with dizziness.
- gammaCore or Truvaga - Any non-invasive vagus nerve stimulation could help if anxiety or migraine is a component.
Some of the effective treatments for vestibular migraine are also effective for PPPD.
Early Diagnosis is Beneficial
Although it can be tough to find a physician who is skilled at distinguishing vestibular disorders and diagnosing PPPD, it appears to be incredibly important to the overall long term success of treatment.
It appears that starting treatment early can lead to a greater benefit long term for the patients and yield a higher success rate. Years of dealing with chronic dizziness can indicate a more severe disability and an acceptance of the illness as everyday life. (Dieterich M, Staab JP, Brandt T. 2016) This is why it’s important to be your own advocate when it comes to your appointments and continue to ask questions. It may even be necessary to travel to find an appropriate doctor, but most often the effort will be rewarded.
More PPPD Information
For more detailed information, see my youtube video on PPPD with Dr. Edward Cho.
References:
- Staab JP, Eckhardt-Henn A, Horii A, et al. Diagnostic criteria for persistent postural-perceptual dizziness (PPPD): consensus document of the committee for the classification of vestibular disorders of the bárány society. J Ves Res 2016
- E J Mahoney A, Edelman S, D Cremer P. Cognitive behavior therapy for chronic subjective dizziness: longer-term gains and predictors of disability. Am J Otolaryngology 2013;34:115–20.
- Dieterich M, Staab JP, Brandt T. Functional (psychogenic) dizziness. Handbook Clinical Neurology 2016;139:447–68.
- Thank you to Dr. Edward Cho from House Clinic for providing some of these materials and clinical experience.


Hello i got PPPD for almost 3 moths now im on SSRI. Is it posaible to fully recover from that its soo bad. I maybe feel a little bit better. What exercise should i do and anything else to help me recover
Hey - it is possible to recover! It can sometimes just take a little while. There are no specific exercises, but movement in general can be helpful. Usually a vestibular therapist can work with you if certain positions are causing an increase in symptoms. But more than that, I'd look into a psychological therapist to help with mindset and different therapy techniques that may help.
Finding this has been very helpful! I've ordered both of your cookbooks which should arrive in the next week or so. I'm a bit stuck and wonder if you might have encountered a bit of a unicorn diet... I'm trying to help a family member who has celiac disease and is a vegetarian and now needs to include low-glutamate due to a recent diagnosis of vestibular migraine and 3PD. The doctor gave a list of foods to avoid and recommended your cookbooks as a starting place. (We live outside of North America with limited access to resources.) My major concern is trying to find more variety of proteins beyond endless cans of beans.
Hi Alicia,
I’ve followed your page for some time. Do you think you had PPPD somewhere in your journey? I had vestibular neuritis and likely PPPD. I’m now finding when I decompensate the PPPD returns. I’m working with my friend physical therapists again. Just curious if you think you recovered from PPPD over time with exercises, life and therapy?
Hey! Yes, we do think that I had PPPD with VM, it just wasnt really diagnosed back when I was diagnosed with VM. I did recover from PPPD with vestibular migraine treatment. Eventually once my attacks calmed, the background dizziness slowly went away.
Hi. My son was recently diagnosed with PPPD. He currently resides in Charlotte, NC and we are having difficulty finding a CBT who has experience with this disorder. Do you know of anyone in his area?
Thanks.
Hey Alvin, I don't unfortunately, I imagine there are very few people. I would recommend reaching out to Kristi (her info is in the post) or Rooted Behavioral Education. Both are vestibular disorder patients who work in counseling! 🙂
I just wanted to say thank you so much to Alicia for posting this, and for everyone above sharing their experiences. I'd never heard of this before but reading through it sounds exactly what I have been suffering with for several years now. The feeling of understanding and possibility that it could be treated is incredible, I could cry. Am going to talk to my doctor about this and hopefully we'll make some progress. Thank you.
I hope you get the answers you need!
i am from mexico am 31 years old now. mexico as been a third world country is hard to find information about this kind of migrane The VM i have a cuestion does your Dc. can treatme by line
sorry for my bad inglish hope a good day for you and your fsmily
Hi Alicia,
I was just wondering if busy environments cause/aggravate dizziness does this necessarily mean you have PPPD? Sorry I know you are not a doctor but you seem very knowledgeable! I am unsure whether I have just vestibular migraine of if I perhaps have PPPD too. Thank you!
No it doesn't. It's common to feel that way with many vestibular disorders. I hope you can get a clear diagnosis soon!
i am from mexico am 31 years old now. mexico as been a third world country is hard to find information about this kind of migrane The VM i have a cuestion does your Dc. can treatme by line
sorry for my bad inglish hope a good day for you and your fsmily
Dear Alicia
I love your website and all the comments from people. These conditions feel like a 'burst golf ball ' inside a tangle of elastic bands of confusion. That's how I feel anyway.
I have had neuritis and being doing VRT for 3 months. I went back to my practitioner who although very knowledgeable and professional is not very 'caring'. He has diagnosed PPPD and sent me away with more exercises. He said not to take SSRI's (recommended by GP) or amitriptyline (recommended by Neurologist) and although I do trust his judgement just don't know which way to turn now as the anxiety has really got a hold.
I asked about diet but he didn't really have any views on it. I really do want to help myself but don't know how. Do you think your diet would help me?
Hey Jill, I would get a second opinion, especially if all he's doing is saying you need VRT. The anxiety is such a normal part so a lot of my friends have done really well with Effexor (even microdosing) to help with the anxiety and PPPD symptoms. I'd recommend seeing a physician who is at least open to trying something else. I believe Dr. Cho and Dr. Beh recommend trying the diet for their PPPD patients, especially if there's a VM component.
Thank you so much Alicia - you are an angel. I think if you get a good doctor then you're more than half way there but unfortunately nobody I've seen has any idea to be honest. You've 'got the tshirt' so really do understand and are so willing to help. So many questions posted on here but you answer everyone so thank you for your care and understanding. If I lived in the states I would definitely go to see Dr. Cho but I will look into the Effexor and try the diet as the head pains, jaw ache going into my ear are very problematic - enough to make anyone anxious. Thanks you so much.
Hi Alicia,
Your website has been so helpful to me! Thank you! I think I have been suffering with PPPD for a long time... probably about 8-10 months or so since my symptoms became bad from VM. However, I was just diagnosed with VM in late april/early May and started treatment. I am starting vestibular therapy this upcoming Friday, two days from now. I am on Topomax, makes me very sleepy! But I am seeing that for PPPD an SSRI or SRNI are more used preventatives. Do you think I should talk to my doctor about changing my preventative or stick to topomax & VRT? I have been on a very low dose of topomax for about 2-2.5 months. I know you are not a doctor, just curious of your thoughts, thanks again for all your helpful tips!!
Hey Cindy, It's a great convo to bring up with your doctor! He may want to add in a med or just see how you do with therapy and the migraine preventative. Sounds like you have a few good things you're starting up and all of this really just takes some time to work. I know we want results immediately!! 🙂 It took me about 4 months to really notice the benefits from the preventative I was on.
Thanks for the really helpful article. Diagnosed with PPPD here.
I'm wondering... is the Heal Your Headache diet recommended for PPPD too? I don't necessarily see how it would help, since there aren't migraine triggers in PPPD... but perhaps it's worth doing anyway? Does Dr. Cho have anything to say about this? I Googled him but couldn't find anything.
I don't want to start cutting foods out unless I have to. With PPPD, the anxiety element means you're always not doing things... and part of CBT for me was encouraging me to do them again. So i don't want to cut out foods unless there's a reason. Or it'll just be more avoidance-behaviours driven by anxiety.
Thanks again for the blog-post!
Hey Dave, If you just have PPPD I don't believe the diet will help. Sometimes there's crossover with VM and PPPD, in which case it would help, but I wouldn't worry about foods and just focus on CBT and getting your exercise/vestibular therapy in. 🙂
Hi Alicia and Dave - Dr. Cho is my Dr. for PPPD and he recommended Alicia's diet 100% and I do believe that it helps to be on it (not as much dizziness), but I can't tell either of you why. Next time I see him, I will talk to him about it further. But Dave, especially now...I would think you could get a video appointment with him.
Thanks for sharing this, Janet!
I have had PPPD for over a year. I do head exercises and have learned how to manage it. Thank God I can only fill it when I am walking and at the end of the day after work. Moving my head from side to side and up and down is a no no unless I do it slowly.. Yes I fill it everyday and some days are worse than others. I am thankful I can function as well as I can.
Dr. Cho is in Los Angeles and specializes in these related disorders. As I mentioned before, I just got lucky when I found him several months into my symptoms, which included episodic chronic fatigue - which he attributed to the PPPD and the exhaustion that comes from trying to feel stable and normal. I highly suggest calling Dr. Cho's office (at the House Clinic in Los Angeles-you can Google it) and ask for a recommendation for a specialist in your area. I have mentioned PPPD to some very sophisticated GP's at the best hospitals and they don't know what it is. As mentioned by Tony, these disorders (vestibular migraines, PPPD, etc.) are newly recognized, most often misdiagnosed, and are complex because they share symptoms. You need a doctor who knows about the disorders. At first another doctor thought I might have Vestibular Migraines but she said that I absolutely needed to see Dr. Cho to figure it out. After conducting the tests, Dr. Cho diagnosed PPPD. And I would say that I am about 75-80% improved since March. PPPD is curable. It isn't always cured, but it is curable. It was Dr. Cho who recommended that I follow Alicia's food plan since an amino acid called tyrosine breaks down into certain foods (becomes tyramine) and is a trigger for symptoms of these disorders. Alicia has a list on her site that you can print out. I think it has made all the difference to eliminate the foods that contain tyramine.
Big fan of him! Glad he's helping you get on the right track! 🙂
This article is interesting as I have been suffering with balance issues since 2010, after witnessing a tragic accident. It was put down to ptsd. I have been experiencing constant symptoms since August 2017 and be given different diagnoses BPPV, labrythintitus, vestibular nutritious have all been mentioned but nothing concrete. I have a new GP who has re referred me to ent as she want a proper diagnosis. My symptoms are pretty much constant but I have adapted my life and just trying to live best I can.
I hope this new GP will have a concise diagnosis for you. I know how tough that can be to not have one that's confirmed.
Hi Alicia,
So glad to see this on your site. While less severe in many ways than the VM's, this is hard to diagnose and I just got lucky, because I ended up with Dr. Cho. My symptoms (since February) have decreased sigificantlty since then. PPPD is also misdiagnosed often, so I got lucky seeing Dr. Cho first off the bat. He's also a nice man.
I will say that the single most effective treatment that somehow works, is also keeping pretty much to you VM receipies.
I hope more people out there get tested for it with a doctor who understands these disorders...
As always, Thank you Alicia - for all you do!!!! The receipes are drool-worthy. LOL.
Janet
Hi Janet,
Has the migraine diet helped with the PPPD or mostly just helped with Migraine? I had vestibular neuritis, probably had PPPD and perhaps a migraine component. Each time I decompensate from the vestibular weakness everything comes back. I haven’t tried the migraine diet for PPPD but I am curious what you have figured out with it.